Project 8p 2022-2024 Research Plan
Project 8p and Perlara started work on the first iteration of the 8p Cure Roadmap earlier this year in parallel with building a preeminent 8p-focused researcher network from the bottom up.
Founded in November 2018 as a 501(c)(3) nonprofit, Project 8p Foundation works to empower a unified community for chromosome 8p heroes for a meaningful life today while accelerating treatments for tomorrow.
Chromosome aberration syndromes such as 8p have long lacked standards of care or approved interventions to lengthen or improve life, and remain understudied for a key mistaken assumption: that because such diseases prove tough to fully model in the lab, and entangle effects of many disrupted genes, they cannot be practically treated, let alone cured.
That misconception lags key advances in genomics and therapeutics. Modern biological understanding and bench methods now extend beyond single-gene/variant diseases, to address scale and complexity of disorders tracing to multiple genes at once, as in long chromosomal aberrations.
And while patients with single-gene disorders such as sickle disease and cystic fibrosis have been first recipients of emerging treatments long deemed science fiction (such as somatic-cell RNA therapy, genome editing, and drug chaperones), genomic methods can now readily detect long chromosome aberrations early enough in development to genomically repair tissues by emerging molecular surgery methods, such as CRISPR-Cas, in time to prevent irreversible damage.
Such early intervention, coupled with effective behavioral therapies to nurture functional plasticity and regeneration, could extend developmental windows later into life to help patients thrive in ways long deemed impossible.
Envisioning that future, Project 8p sees a path from today’s absence of treatments to a set of reliable cures for anyone on earth with a molecularly confirmed clinical diagnosis of rearrangement (inversion or translocation) or aberrant segmental copy number (CNVs) in the short arm (p) of chromosome 8.
That big tent includes 8p heroes with deletions/duplications/inversions/translocations (del/dup/inv/tran), deletions (del) only, and duplications (dup) only. Effects of such aberrations vary in ways already partly known: 8p heroes with complex rearrangements, or long deletions nearer the chromosome 8 centromere, tend to have the most severe clinical presentations, for example.
But despite such variability, 8p families form not just a list of n-of-1’s, but a natural coalition whose overlapping experiences can help trace particular symptoms to particular targetable genes, so that families mutually benefit by pooling effort and insights from their respective journeys.
More than 500 known patients worldwide endure such varied chromosome 8p syndromes. While many suffer congenital heart defects and other lifelong organ deficits, Project 8p first aims to rescue early-life neurological development, while laying groundwork to reduce cognitive, neuromuscular, cancer, and other risks as 8p heroes grow to adulthood.
Our next two years will aim to i) identify candidate early-life neurological therapies via parallel-assay drug repurposing, ii) appropriately match the most promising such candidates to appropriate patients for urgent compassionate trial, and iii) apply findings to guide further development of drug and molecular surgery-mediated cures for families in the future.
To achieve that aim of effectively treating symptoms in some patients by 2024, Project 8p must transcend conventional approaches limited to one or few notional driver genes whose effects may not be directly therapeutically modifiable. Instead, we will apply robust modern methods of comprehensively quantifying the activity of many genes at once, in equivalent tissues of each patient, to build an informative, minimally biased assay for distinctive tissue function states in 8p heroes with similar or distinct chromosome 8p aberrations.
Funding Strategy
Within a community of family, care, and research stakeholders, Project 8p Foundation spearheads translational work by directly seeding bench research in university labs, conditioned on data sharing and community service, with follow-on funding via multi-PI grants and outside gifts.
Our two-year plan aims to generate and leverage promising data without ceding governance or urgency, by i) teaming with CZI Rare As One grantee foundations to convene scientists in a shared incubator lab where patient families drive research aims and own materials and intellectual property; and/or ii) extending the Chordoma Foundation’s CF Labs model to establish a dedicated co-lab for driving preclinical research on the most feasible and 8p-applicable therapeutic modalities.
Project 8p has seeded, and will further support, drug repurposing by parallelized assays of individualized cell lines from 8p heroes, to stabilize and potentially improve life quality even before statistically tracing particular disease states to particular 8p genes. Importantly, such parallelized drug assays intrinsically help characterize cellular disease phenotypes, and (via genetic modifier screens) how they depend on patient genetic variation – which can, in turn, help identify unexpected disease modifiers and drug targets.
As in hero and in vitro data grow, computational modeling of etiology will become more informative, letting us statistically prioritize candidate genotype-phenotype relationships to validate among our several hundred already engaged 8p heroes, as well as those we recruit anew. With genomic and epidemiological data suggesting several hundred undiagnosed 8p heroes in the US alone, Project 8p has a strategy to help regional and nationwide hospital systems identify them in time to repurpose drugs to manage and stabilize early-life neurological development.
Project 8p will also spearhead pilot test programs of augmentative medical devices, e.g., brain-computer interfaces, and assistive technologies that are currently applied in the rehabilitation of traumatic brain and spinal cord injuries. In parallel, we aim to refine emerging cell- and chromosome- therapies for curative intervention in their and others’ lifetimes.
Chromosome Pioneer
Project 8p thus stands uniquely ready to serve as a pioneer chromosome disorder, clearing a path for other chromosome disorders to follow. Despite the pandemic, Project 8p has spent its first three years building the following foundational Accelerated Research template:
a global patient registry and centralized biobank of patient-derived blood cells and fibroblasts poised for iPSC reprogramming and distribution to researchers
an ongoing longitudinal natural history study paired with biosample collections linking clinically observed data and EHR records
a foundational representative inv/dup/del 8p family trio dataset spanning chromosome breakpoint analysis to iPSC micropatterning assay to brain organoid multi-omics characterization
a collaborative network of cure-focused researchers who are eager to be put to work with Project 8p funding and project management support
Including launching a Commission on Novel Technologies for Neurodevelopmental Copy Number Variants (AJHG, Aug 2022)
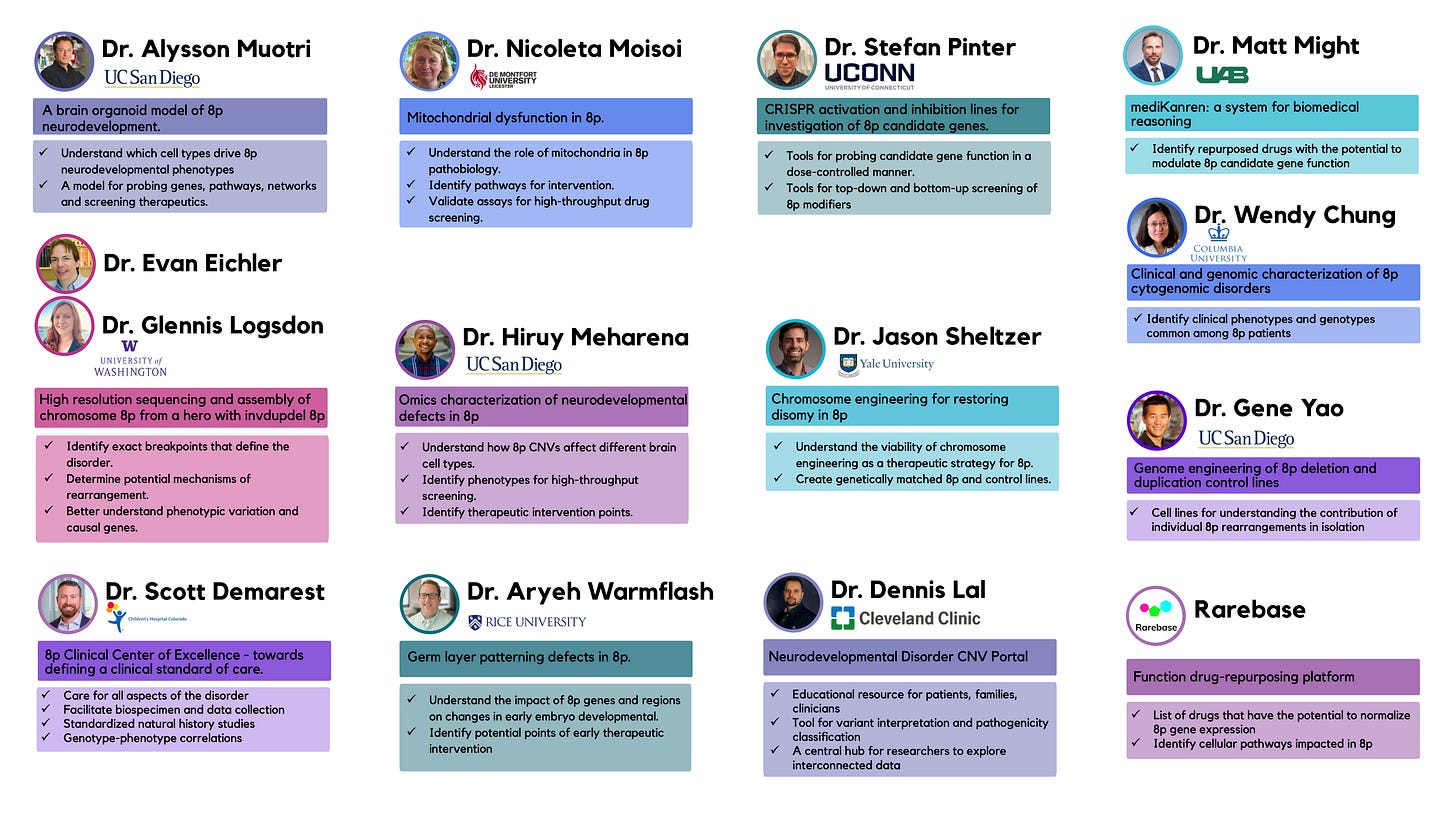
The growing nucleus of the Project 8p researcher community unites:
Dr Alysson Muotri (UCSD)
Dr Glennis Logsdon (University of Washington)
Dr Evan Eichler (University of Washington)
Dr Jason Sheltzer (Yale University)
Dr Hiruy Meharena (UCSD)
Dr Dennis Lal (Cleveland Clinic and Broad Institute)
Dr Stefan Pinter (University of Connecticut)
Dr Nicoleta Moisoi (Leicester School of Pharmacy)
Dr Aryeh Warmflash (Rice University)
Drs Matt Might and Andrew Carouse (University of Alabama)
Drs Whitney Dolan, Nathaniel Pearson, Travis Zack and Ethan Perlstein (Perlara PBC Cure Guides)
Rarebase PBC
Key Opinion Leaders from the (8p Founded) Commission on Novel Technologies for Neurodevelopmental Copy Number Variants and respective Steering Committee (Dr. Dan Lowenstein, Dr. Anthony Wynshaw-Boris, Dr. Heather Mefford, Dr. Alysson Muotri)
Project 8p Medical & Scientific Advisory Board (Dr Wendy Chung, Dr Scott Demarest)
Scientific progress and plan
Project 8p’s 2021 Five Year Strategic Plan specified core scientific resources and milestones, three of which we have now achieved by i) establishing a Neurogenetics Multidisciplinary Clinic scalable model; ii) opening a catalytic research program (seeded by Global Difference Makers pledge) to pioneer 8p families, scientists, and sponsors; and iii) generating hero-family trio iPSC pilot findings (Okur et al., 2021; Logsdon & Eichler, in prep.; Warmflash, in prep.) whose four key lessons anchor our research plan:
Conventional candidate/driver gene approaches fail in 8p syndromes, as each hero’s multi-gene lesion reverberates distinctively, through diverse tissues, over life. As such, following disease courses in many enrolled 8p heroes can clarify which outcome-informative biomarkers to model in the lab – and how. Put simply, to make in vitro meaningful, start in hero.
Among 8p symptoms, early childhood neurological dysfunction crucially gates life length and quality, so naturally merits first focus. Prioritizing young heroes to characterize and neuronally lab-model can identify genes targetable both individually and across young heroes – and perhaps also in later-life dysfunction of brain and other tissues, as footholds to further therapy development for ever more patients. As such, we will longitudinally profile hero-specific neuronally differentiated iPSC organoids, to identify plausible targets for early-life intervention.
To efficiently identify potential therapies in such organoids, we will parallelize organoid responses to existing drugs (typically, but not necessarily, small-molecule) active in plausibly 8p-relevant cellular biochemistry and downstream tissue function and development.
Longer term, to better profile 8p heroes and develop good therapies for more of them, we will harness emerging chromosome- and cell-specific assay/intervention methods, including antisense oligonucleotide regulation (to modulate specific gene expression); chromosome-specific therapies (to silence and/or repair 8p lesions); cellular regeneration and rejuvenation (to avert, stop, and/or reverse tissue damage); and whole-tissue repair or replacement (by antigen-matched allogeneic, kin, or self iPSC-derived antigen-matched tissues).
In key background work, Project 8p scientific advisor Wendy Chung and colleagues identified several previously functionally assayed genes on the short arm of chromosome 8 that likely figured in disease course in one or more of 97 studied heroes (Okur et al., 2021).
Crucially, these findings showed how little such known lamp-post genes yet explain: nearly a third of studied heroes with no structural lesion in strongly penetrant GATA4, for example, nonetheless developed congenital heart defects; so while GATA4 may often drive congenital heart defects in 8p, other yet unspecified local genes likely matter as strongly.
These findings hint that 8p heroes’ diverse complements of affected genes – and of cis-regulatory expression-relevant lesion topology – lack the monogenically gated etiology of some other syndromes (e.g., SHANK3-driven Phelan-McDermid or UBE3A-driven Dup15q), and instead may foundationally exemplify the variable, multi-gene etiology typifying most gross chromosomal syndromes.
Crucially, such complexity can readily involve interaction among dosage-sensitive linked genes (and likewise allelically varied genes on other chromosomes) – as in autism spectrum presentations traced by Project 8p’s Alysson Muotri and colleagues to varied aberrations of chromosome 16p11.2.
That work identified no clear local driver gene, but, via pathway analysis, revealed that both dup and del 16p11.2 lesions can impair neuronal migration via overactive RhoA signaling – which, strikingly, pharmacological intervention could rescue (Urresti et al. 2021).
We thus aim to transcend limitations of candidate gene approaches by embracing and leveraging heroes’ genomic and phenotypic diversity, to efficiently find targetable causal footholds. Putting our dollars to work directly studying more of the world’s 8p heroes, by comprehensively profiling in vivo disease course and efficiently parallel-assaying in vivo drug response, may yield the fastest useful insights for individuals and, ultimately, cohorts.
In addition to quickly scaling the set of known 8p heroes with long-term health data, we will follow up bioinformatically, experimentally, and clinically to assess candidate causal genes – including by assaying potentially definitive etiology in rare individuals with nulli-, mono-, poly-, or uniparental isodisomy of particular 8p genes.
Within five years, we aim to standardize protocols for clinician-investigator-led pioneer trials (each in one or few heroes) of compelling drug-repurposing candidates, medical devices and newly maturing chromosome/cell therapy modalities (e.g., antisense oligonucleotides, siRNA cocktails, and genome editing) to health-tune relevant gene expression and function in heroes of 8p and, for groups following the path we blaze, other syndromes.
These pioneer trials will anchor the broader survey of disease courses in yet more heroes, eventually allowing more statistically robust multi-center insights on biomarkers and outcomes – and, in the ultimate phase, broader clinical trials and sustainable biotech development needed to bring reliable cures to families worldwide.
Decision-making
From 2018 to 2021, Project 8p conducted a scientific review to identify and seed-sponsor pioneer researchers and clinicians advancing the four research segments detailed below. Proposal solicitation for the first half of 2022 anchored the network with our current six founding research groups.
With that braintrust in place, we plan a virtuous circle to grow expertise and insights, by asking Project 8p-funded principal investigators to review new proposals (except where recusal is appropriate) and agency requests for proposals. Such community service extends the anchor engagement of our 8p Researcher Roundtable, which monthly gathers 8p families and Project 8p-funded researchers and clinicians for robust exchange of phenotypic insights from patient care circles, and science updates and brainstorming by and for labs.
For 2022-2024, engaging Project 8p-funded scientists to assess proposals and new potential collaborators efficiently advances our communal mission and esprit de corps.
As preclinical research transitions to clinical development and commercialization, and the funding requirements increase significantly, Project 8p will consult with members of the Project 8p MSAB as well as external experts retained on a project basis to critically assess the following:
Mission relevance
Scientific validity, feasibility, and ceiling utility
Complementarity with other Project 8p research
PI expertise
Capital needs in milestone based approved budget
Path (budget and timeline) to clinical proof-of-concept
Drug development strategy
Role of venture philanthropy and value of IP promise
Segment 1 - DRUG REPURPOSING
Parallelized, AI-informed Drug Repurposing
Our search for 8p treatments anchors in high-throughput, bias-minimized phenotype-rescue drug repurposing, in three 8p-hero-derived tissue types: fibroblasts (for baseline structural/functional and cross-tissue insights); iPSC-differentiated neural progenitor cells (for lineage-specific developmental insights); and iPSC-differentiated excitatory neurons (for insights on differentiated tissue dysfunction). In parallel, we aim to leverage ancillary insight from patient-reported outcomes, partnered academic projects (some using machine learning to mine multimodal findings), and data-grounded, physician-initiated off-label n-of-1-or-few trials.
Starting with pilot findings from an inv/dup/del family trio, 8p-hero-derived primary fibroblasts will be assayed with a standardized, validated panel of dyes targeting mitochondria, nuclei, and other organelles/cell compartments (cell painting). Growth under challenge (e.g., on galactose without glucose, or in presence of DNA damaging agents) will help identify potential rescue drugs. Ideally, many assessed phenotypes in 8p fibroblasts may statistically differ in patients versus controls – perhaps with one or more robust mitochondrial and/or nuclear disease phenotype that can be ameliorated in a 96- or 384-well-plate screening assay optimized in the lab of Professor Nicoleta Moisoi at the Leicester School of Pharmacy. The Broad Repurposing Hub (REPO) libraries and/or ReFRAME collection could then be screened.
After validating the Cell Painting workflow on 8p fibroblasts, the same workflow will be applied to 8p iPSC-differentiated neural progenitor cells. Assuming recent findings involving trisomy 21 patient cells translate to 8p patient cells, (Meharena et al., 2022), we recommend screens on 8p iPSC-derived neural progenitor cells using an image-based/high-content nuclear membrane (lamin) visualization assay to identify repurposable drugs that rescue senescence-associated nuclear membrane defects, specifically loss of lamin staining. In an ideal case, 8p neural progenitor cells exhibit a robust nuclear membrane morphology disease phenotype that can be reversed or ameliorated in a 384-well-plate screening assay developed and optimized in the lab of Prof Hiruy Meharena, followed by screening of the Broad REPO libraries and/or the ReFRAME collection.
In an ongoing project with Rarebase, the FUNCTION platform is using 8p iPSC-differentiated NGN2+ excitatory neurons to identify repurposable drugs that increase expression of haploinsufficient genes, i.e., deleted 8p genes with an intact second copy, and rescue eventual electrophysiological deficits. Rarebase is also performing a CRISPR mutagenesis screen to identify disease modifiers of 8p that are shared by other neurodevelopmental disorders. The final data report is expected in Q4 2022. If the results are promising, additional funds will be allocated for assembling a preclinical data package including hit validation and mechanism of action studies.
To complement the empirical, experiment-based approaches, the last type of unbiased drug repurposing is AI-based. In collaboration with the University of Alabama’s Institute for Precision Medicine under the leadership of Professor Matthew Might’s team, we recommend reengaging with the MediKanren team to see what drug repurposing recommendations can be generated by AI from the medical literature. Working with the MediKanren group will not require initial funding from Project 8p; however, in the event that one or more promising clinical candidates or therapeutic mechanisms of action are identified, there will be costs associated with preclinical followup work and with launching single-patient pioneer IND studies (Might and Crouse, 2022).
An initial trial was performed in Q2 2022 with a 8p gene set consisting of five deleted/monosomic genes and two duplicated/trisomic genes: CSMD1, DLGAP2, ANGPT2, CLN8, MCPH1, RHOBTB2, CHRNA2. No clinically actionable hits or pharmacological classes were identified on this first pass.
Segment 2 - In Vitro Modeling
Disease in a Dish & Therapeutic Target Assessment
The advantage of unbiased drug repurposing screens is that they don’t require complete knowledge of the underlying disease mechanism. As we’ll discuss in Segment 3, targeting root causes of 8p disorders entails fixing and/or replacing damaged chromosomes, which drive chronic tissue stress even after neurodevelopment. The goals of this Segment are discovery of disease-modifying drug targets and aneuploidy-compensating pathways like the integrated stress response (ISR), which will provide added and in some cases significant therapeutic benefit above what will be provided by repurposed drugs.
We envision disease modeling using three 8p-hero-derived cell types of increasing complexity: iPSC-differentiated neural progenitor cells (NPCs), iPSC-differentiated excitatory neurons (iNeurons), and iPSC-differentiated brain organoids.
Professor Hiruy Meharena’s lab at UCSD will investigate the transcriptome using RNA-seq, the epigenome using ATAC-seq, and the 3D-genome using Hi-C of 8p iPSCs and NPCs. The Meharena lab will interrogate the consequences of invdupdel(8p) on the integrity of the nuclear architecture through confocal microscopy of the epigenome and nuclear envelope, and assess if these features are associated with senescence. Based on the clinical manifestation of invdupdel(8p), it is hypothesized that neural progenitor cells (NPCs) will be sensitive to genomic imbalance of chromosome 8p.
In an ongoing collaboration with Prof Alysson Muotri’s lab at UCSD, 8p brain organoids are currently being differentiated from the pathfinding inv/dup/del family trio iPSC lines. These personalized 8p organoid models will serve as the in vivo surrogate model for validating disease modifiers that emerge from disease modeling or in hero studies. The goal is to generate and characterize brain cortical organoids from a 8p proband and their respective biological parents. Brain organoids will be produced from human iPSCs using the protocol developed by the Muotri lab. During early stages of the brain organoid generation, Muotri lab will compare parents vs. proband on cell proliferation, cell death and synaptogenesis to identify informatively screenable cellular phenotypes. Such cellular phenotypes could be used to screen drugs or test other therapeutic options as next steps. A global gene expression assay will be performed to detect eventual neurodevelopmental molecular pathways that are altered at this stage. To identify genes that are misregulated in different cell types, they will perform single cell RNAseq on long-term brain organoids (8-9 months). At this stage, brain organoids contain the major classes of brain cells (excitatory neurons, inhibitory neurons and glia), allowing them to determine which cell type is driving potential phenotypes.
As examples of current leaders in the space, Rumi Scientific or Vyant Bio, biotech companies that specialize in high-throughput analysis and screening of brain organoids (neuroloids), may be engaged to validate hits from iPSC-based drug repurposing screens once 8p brain organoids have been fully characterized by the Muotri lab.
We have also conducted an internal driver-gene analysis using public data and a combination of public and private bioinformatics and artificial intelligence tools. In brief, for each patient in the largest public 8p clinical dataset, we have analyzed all deleted and duplicated genes in conjunction with their clinical symptoms, identifying the genes that appear most strongly associated with their symptoms in the clinical literature. We have integrated these results with prior review by 8p experts, and identified 4 genes that we recommend be prioritized for further analysis: CSMD1 (a tumor suppressor gene), DLGAP2 (an autism-associated synaptically expressed gene), MCPH1 (Microcephalin), and ANGPT2 (Angiopoietin 2). Each of these genes has been deleted in large numbers of patients (>60 in the Okur et al cohort), including the pathfinding 8p trio, and is supported by some combination of published literature and genomic instability in public databases.
Prof Aryeh Warmflash’s lab at Rice University has developed experimental methods to model neurodevelopmental defects using the iPSC micropatterned differentiation assay, which can be used to understand how the mutations associated with 8p affect signaling and cell fate decisions during early development. The Warmflash lab will use the iPSC micropatterned differentiation assay to check for relevant phenotypes in multiple 8p iPSC lines, and in parallel will assess the effects of deletion or duplication of two candidate neurodevelopmental 8p driver genes.
Follow-up combinational analyses can expand to additional predicted driver genes in the deleted regions, and eventually screen the knockout, down-regulation or up-regulation of every gene in the short arm of chromosome 8p in brain organoids in high-throughput functional assays in collaboration with a partner like Rumi Scientific or VyantBio. In theory, 8p heroes who are diagnosed in the first few years of life could be treated with combinations of experimental ASOs that are discovered and validated using personalized brain organoids.
Segment 3 - Cell and Chromosome Therapies
Building the foundational toolkit
As both a hedge and a complement to Segments 1 and 2, we recommend collaborating with multiple academic groups (and if possible early-stage biotech startups) on current and emerging modalities that are CNV-agnostic. As stated several times above, the rationale for focusing on the root cause of 8p disease – damaged 8p chromosomes – is that it obviates the need to validate driver genes one by one.
As an initial down payment on the promise of chromosome therapy, Project 8p will sponsor a diversified five-pronged approach in the lab of Professor Jason Sheltzer at Yale University in order to identify techniques that restore 8p disomy (i.e., a normal diploid karyotype) in the pathfinding inv/dup/del pioneer proband. The first approach involves simply growing 8p iPSCs in the lab over many generations (cell divisions) and checking for spontaneous loss of the damaged 8p chromosome, as has been previously demonstrated to happen with Down Syndrome iPSCs. The second approach is an accelerated form of the first approach that involves treating 8p iPSCs with a drug that increases the rate of spontaneous loss of damaged 8p chromosomes. The third approach uses CRISPR (gene editing) to target DNA sequences specific to damaged 8p chromosomes, resulting in their physical elimination from the cell. The fourth approach also takes advantage of CRISPR but instead of targeting naturally occurring sites unique to damaged 8p chromosomes, a susceptibility gene is inserted into the damaged 8p chromosomes of 8p iPSCs, rendering these edited cells sensitive to a drug that selectively kills them. The fifth approach involves a technique called microcell-mediated chromosome transfer (MMCT) whereby a second copy of a normal 8p chromosome is delivered to 8p iPSCs, followed by application of the four preceding approaches on trisomic post-MMCT 8p iPSCs to restore a normal karyotype.
If any of one or more of the five approaches succeeds in yielding restored-disomy cells, the proliferative rate, RNA-seq/transcriptomic profile and differentiation capability of restored-disomy cells will be measured in comparison to the original 8p-rearranged cells. From a practical standpoint, restored-disomy cells will also serve as an isogenic-corrected control in any in vitro experiment. Right now no such isogenic-corrected control lines exist.
Professor Stefan Pinter has proposed to build inducible CRISPRi (gene inhibition) and CRISPRa (gene activation) constructs into a euploid (46,XY) human induced pluripotent stem cell line, which will be further equipped with an inducible NGN2 transgene for rapid neuronal differentiation. In parallel, the Pinter lab will build an equivalent 8p-relevant reference hiPSC line by introducing the dox-inducible NGN2 construct as well as a CRISPRa/i construct into the inv/dup/del line, which will enable both bulk and single-cell RNAseq comparisons of euploid vs. inv/dup/del hiPSC-derived neurons.
Because many chromatin loops anchor with vital DNA strand polarity, segmental rearrangements can change how promoters and enhancers regulate 8p genes. In neurotypical cerebellum, such dispersed elements regulate key genes in segments of 8p subject to inversion or other rearrangement, suggesting that rearrangement-disruptable enhancers may crucially regulate multiple syndrome-intrinsic genes. In the context of inv/dup/del, the copy-number neutral inverted segment is also neutral with respect to its gene dosage, because these enhancers would also have been deleted on the inv/dup/del allele. For this reason, the Pinter lab will build flexible experimental tools that enable dissection of a broader list of candidate genes that could be narrowed as gene expression data from relevant cell types across 8p hero cohorts, including the inv/dup/del hiPSC trio, become available.
The CRISPRi and CRISPRa lines to be generated by the Pinter lab will complement a related effort by Rarebase who utilize a commercial hiPSC line with inducible NGN2 but constitutive CRISPRi. Inducible CRISPRi & CRISPRa lines will enable alteration of gene dosage before or after neuronal differentiation, and additionally test which cellular phenotypes remain reversible in post-mitotic neurons.
Segment 4 - In hero Studies
In hero studies to elucidate disease drivers and prototype augmentative therapies
Segment 4A
Project 8p will continue to fund efforts to identify and recruit 8p heroes into the IRB-approved Chromosome 8p Registry and Biorepository led by principal investigator, Bina Shah, CEO of Project 8p in an effort to be agile with a sense of urgency. This is the start of a robust and standardized retrospective and prospective natural history study.
Segment 4B
Project 8p will engage with cutting-edge biotech startups developing brain-computer interface devices, neuromodulation, or assistive technologies to explore pilot programs that will give 8p heroes access to experimental augmentation therapies.
Segment 4C
Building on those efforts and as a way to link in vitro disease modeling results to phenotypic information about 8p heros, we recommend exploratory clinical biomarker discovery studies of 8p hero biosamples using assays such as the Nomic Bio nELISA proteomics platform that measures hundreds of secreted protein levels.
Segment 4D
In collaboration with Drs. Evan Eichler and Glennis Logsdon, we strongly recommend applying the new genome assembler and long-read sequencing to build reference genomes for additional 8p family trios to identify potentially pathogenic rearrangements. We will integrate genetic, transcriptional, and epigenetic data to understand the genes and pathways affected in each patient. Ultimately, a comprehensive meta-analysis of these data will reveal pathways of genomic pathogenesis. This may reveal never-before-seen complex SVs, provide the most detailed view of the genetic content of genomes associated with neurodevelopmental-related disorders, and help explain the genetic basis for phenotypic variation associated with 8p disorders. The hope is that it spurs the development of new methods to better characterize families at the genetic and genomic level and, importantly, suggest new hypotheses for the diagnosis and treatment of these disorders.
In order to assess the presence of previously unresolved duplications flanking the megabase 8p inversion. We also recommend assessing the effects of SNPs and variants (or CNVs) outside of the 8p region and how they interact with the 8p lesion.
This work could also be complemented by an unbiased, CRISPR-based screen for genes that bypass the impact of the CNV and rescue the phenotypes of 8p-hero-derived cells.
Segment 4E
With the launch of the first Neurogenetics MultiDisciplinary Clinic at Children’s Hospital of Colorado, a coordinated team of clinical providers are able to observe and treat 8p heroes over time, as well as enroll them into research in order to link clinical data at point of care in a systematic and standardized way to patient reported data in the Chromosome 8p Registry. The goal is to expand this model towards additional hospital clinics towards deep phenotyping of patients with informative genetic variation, and the connection and movement of that data with biosamples and derived tissues. This will contribute substantially towards a quality standard of care and support researchers and inform investigator priorities as partners to our precious seed investments.
Unfortunately, clinical, genetic, and molecular data are currently siloed across disparate laboratories, registries, databases, and the literature. Therefore, the CNV Commission has established a ‘‘Clinical Research Data Platform’’ to collect and link new and existing data elements from consented individuals with the biorepository. This data platform facilitates genetic diagnosis interpretation, research, and education for CNVs/SVs. Importantly, this platform structure also facilitates the sharing of relevant information back to the participant. Robust governance and machine-readable sharing preferences enable expedited sharing of data on the basis of patient consent.
Moreover, hospital systems are an untapped well of undiagnosed 8p heroes, specifically patients who have failed WES or have only been tested using microarray hybridization based screening for CNVs. In parallel collaborations with Prof Dennis Lal at Cleveland Clinic, we recommend identifying patients with monosomy or trisomy of an 8p gene and determining if their phenotypes match those of 8p heroes whose lesion includes said 8p gene.
This information could add insights into driver genes. Moreover, we are interested in recruiting additional patients to the Chromosome 8p Registry if contactable via the EHR/EMR systems and finding older 8p heroes to understand prognosis well beyond adulthood. This will inform research priorities and contribute to a better understanding for an improved standard of care.
From Discoveries to Drugs
Project 8p envisions a stepwise transition from an academic-directed albeit foundation-sponsored research model to a community-directed and foundation-sponsored research model where clinical translation projects are advanced exclusively in 8p-dedicated lab space (8p Labs, Inc.) by 2024.
Since the start of 2022, Project 8p has in place a distributed and capital-efficient team that manages external research projects, maintains community engagement, and oversees day-to-day operations. The 6 labs funded in 2022 will bear fruit in the form of assays, tools, cell lines and lots of data throughout 2023.
In the ideal scenario, Segment 1 will create a drug repurposing to drug discovery pipeline that yields one or more drug repurposing clinical candidates that can be evaluated for safety and efficacy in single-patient pioneer studies starting in the second half of 2023.
In the ideal scenario, Segment 2 will create a trove of valuable data yielding targets and pathways that are therapeutically modifiable early in life while the neurodevelopmental window is still open.
In the ideal scenario, Segment 3 will demonstrate that chromosomal surgery is possible in cells in a dish, and the community will have the tools to target discrete sets of disrupted 8p for therapeutic rescue by programmable nucleic acid medicines.
In the ideal scenario, Segment 4 will add a first line of treatments and interventions that will positively impact quality of life for 8p heroes as well as lead to the creation of a vibrant online portal for navigating the trove of data and outputs across all four Segments, creating a clinical trial flywheel in the second half of this decade (2025-2030).
Project 8p will use the second half of 2022 to evaluate venture philanthropy and drug development models that could be borrowed by other CNV communities, including the following:
nonprofit biotech: Cure Rare Disease (Rich Horgan) developing a CRISPR therapeutic for Duchenne muscular dystrophy
Public Benefit Corporations (PBCs): Perlara and Rarebase
Program-related investments
Shared Resources for Stronger Team Science
Project 8p’s role in the CNV Commission
In 2020, the Chan Zuckerberg Initiative selected Project 8p as a rare disease grantee to launch the Commission on Novel Technologies for Complex Copy Number Variants. With two other patient groups as partners (Dup15Q Alliance and Ring 14 USA), the CNV Commission is a patient-led consortium that is developing shared infrastructure and prioritizing treatments for those with neurodevelopmental chromosome disorders caused by CNVs or structural variants.
The confluence of clinical phenotypes across many neurodevelopmental CNVs implies convergence in at least some aspects of the underlying genomic mechanisms. We want to approach neurodevelopmental-related CNVs/SVs as a class of disorders that can be identified, investigated, and treated on the basis of shared mechanisms and/or pathways (e.g., molecular, neurological, or developmental). We articulate a clear vision for piloted roadmap strategies to reduce patient/caregiver burden and redundancies, increase efficiency, avoid siloed data, and accelerate translational discovery across CNV/SV-based syndromes.
A recent partnership amongst Illumina, the Commission on Novel Technologies for Neurodevelopmental Copy Number Variants, and RARE-X will collaborate to generate whole genome and whole transcriptome sample data of individuals diagnosed with rare neurodevelopmental disorders caused by copy number variants (CNVs) or structural variants (SVs). Through this project, the collaborators aim to understand the utility of next-generation sequencing technologies in analyzing the effect of large CNV or structural variants in neurodevelopmental disorders.
Project 8p is eager to continue supporting the infrastructure for this but will depend on external funding sources to be excited about this opportunity to invest in the Commission.